Introduction
If you’re a man over 30 and have noticed an uptick in digestive issues like constipation, bloating or diarrhoea, low testosterone levels could be the culprit.
As an important male sex hormone that plays a key regulatory role across body systems—including gastrointestinal functioning—deficient testosterone is increasingly linked to bowel movement difficulties.
Multiple clinical studies demonstrate that declining testosterone often manifests through digestive problems like constipation as cells become less responsive and muscles weaken over time.
Constipation refers to an infrequent, difficult passage of stools—less than three times a week—wherein faeces are hardened due to excess water absorption in the colon.
This troubling symptom not only causes substantial discomfort but can negatively impact health in numerous ways when unchecked in the long term.
Fortunately, getting tested and addressing low testosterone levels through medical or lifestyle approaches can help resolve testosterone-related constipation while restoring wellness more broadly.
Inside this comprehensive guide for men, learn:
- How common hormone deficiencies connect to functional issues like constipation
- The role testosterone plays in healthy digestion and regular bowel movements
- Specific causes, symptoms and risk factors for low testosterone constipation problems
- Available medical exams and lab work critical for an accurate diagnosis
- Overview of prescription and natural treatment options to know
- Key lifestyle changes to improve low testosterone and alleviate associated gastrointestinal problems
Understanding the scope of this issue begins with appreciating prevalence across demographics.
Do read the People Also Ask (FAQs) about this topic.
Key Takeaways
- Testosterone plays a crucial regulatory role in healthy digestion and bowel movements. Deficient levels lead to reduced nerve sensitivity, weakened intestinal contractions, painful cramping, bloating, and constipation.
- Multiple studies show that low testosterone manifests in the form of gastrointestinal issues like infrequent, difficult defecation and irregular bowel movements.
- Getting tested for low testosterone is important if you have digestive complaints like constipation, diarrhoea, nausea, and haemorrhoids that are unexplained. A blood test remains the gold standard for accurately measuring deficiency.
- Addressing low T through medications like testosterone replacement therapy or secondary gonadotropin drugs can alleviate related gastrointestinal problems, restoring regularity often within weeks.
- Certain lifestyle measures like reducing sugar, minimizing stress, and optimizing sleep and activity levels have research confirming benefits for improving testosterone levels and digestion simultaneously.
Prevalence of Low Testosterone
After age 30, men’s testosterone production naturally declines at a steady rate of about 1 per cent annually.
Chronically deficient levels qualify as low T or hypogonadism when total blood concentration dips below 300 nanograms per deciliter (ng/dL).
According to a wide body of research, this includes:
- 2.1 percent of men in their 40s (Johns Hopkins Medicine)
- 3.2 percent of men in their 50s
- 5.1 percent of men in their 60s
- 50 percent of men in their 80s
Furthermore, vitamin D deficiency—very common in older males—can accelerate testosterone depletion by up to 25 percent while indirectly harming cellular health.
Notable drivers of premature or accelerated testosterone loss extend beyond ageing itself to include:
- Genetic conditions (e.g. Klinefelter syndrome)
- Pituitary tumours
- Chronic illnesses (e.g. type 2 diabetes, AIDS)
- Obesity
- Sleep apnea
- Inflammation
- Injury or infection impacting testes
- Damage from drugs, toxins or radiation
- Stress
- Zinc deficiency
As experts clarify, “Low testosterone, or low T, is diagnosed when levels of testosterone in the blood are below 300 ng/dL.”
Hallmark signs span sexual dysfunction, depressed mood, fatigue, shrinkage of testicles and muscle loss.
Now what does this have to do with constipation and other digestive troubles?
The Gut-Testes Connection
Research increasingly illuminates a bidirectional, interdependent relationship between balanced testosterone function and healthy digestion dubbed the gut-testes axis.
This refers to the endocrine system communication pathway between sex hormones and the enteric nervous system lining the gut.
Here’s how it works:
The hypothalamus gland secretes gonadotropin-releasing hormone in the brain to signal the pituitary gland to manufacture luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
LH and FSH then prompt specialized Leydig and Sertoli cells within the testes to ramp up testosterone production which enters circulation to spur masculine developmental changes.
Concurrently, trillions of beneficial bacteria comprising the intricate gut microbiome help convert precursor steroids into usable testosterone while regulating inflammation.
When operating optimally, enzymes and proteins throughout the digestive tract also deactivate excess testosterone and prevent unhealthy conversion into DHT or estrogen.
However, in cases of chronic gut flora imbalance (dysbiosis), infection, small intestine bacterial overgrowth (SIBO) or low stomach acid, this leads to deficient testosterone.
Likewise, poor gut health paired with declining testosterone hinders the strength of intestinal contractions and transit speed—frequently causing constipation along with diarrhoea, cramping or nausea issues.
Now that you understand the gut and endocrine relationship scientifically, let’s break down the digestive roles of testosterone more clearly.
Testosterone Deficiency Causes Constipation: How?
This vital sex hormone contributes to bowel regularity and easier passing of stools through various gastrointestinal mechanisms:
- Stimulates pelvic floor nerves to effectively coordinate downward contraction and relaxation of relevant muscles.
- Regulates water content absorption across colon walls.
- Fuels muscle growth including intestinal linings.
- Controls inflammation and gut barrier integrity.
- Shapes microbiome diversity which aids digestion.
However, shrinking levels lead to reduced nerve sensitivity, weakened intestinal contractions, painful cramping, bloating and constipation.
A lead researcher summarizes, “Low testosterone seems to cause reduced mobility and transit speed through the digestive tract leading to functional issues like difficult defecation and irregular bowel movements.“
Now what does testosterone deficiency constipation feel like?
Signs and Symptoms
If aggravating symptoms below sound familiar paired with unchanged diet and fluid intake, hypogonadism could be the issue:
- Passing less than three stools per week
- Hard, dry, pebble or pellet-like stools
- Straining excessively to eliminate faeces
- Incomplete bowel movements with a sense of obstruction
- Bloated sensations and visible abdominal swelling
- Generally infrequent or absent urge to defecate
- Increased intestinal gas
- Acute pain or soreness during elimination
Secondary symptoms also often emerge over time like:
- Hemorrhoid development
- Anal fissures
- Bowel leakage
- Rectal prolapse
Testing is imperative whether you only display digestive difficulties or a range of traditional low T red flags.
Risk Factors to Know
Multiple risk factors and underlying health conditions can deplete testosterone stores—indirectly promoting constipation—such as:
- Obesity and associated inflammation
- Chronic stress exposure
- Smoking cigarettes or abusing other drugs
- Excess alcohol consumption
- Lung disease or sleep apnea
- Cancer treatment (chemotherapy or radiation)
- Spinal cord injury
- Pituitary disorders
- Certain rare autoimmune conditions
Testing is essential to pinpoint the clear catalyst while ruling out other possible gastrointestinal maladies driving constipation like IBS or Crohn’s disease.
Diagnosing Low Testosterone as the Culprit
Don’t gamble with assumptions. Work directly with an experienced men’s health, urology or endocrinology specialist for accurate diagnosis through two avenues:
Physical Exam Assessment
This begins with an in-depth review of personal and family medical histories involving related issues followed by a physical to check for:
- Penile discolouration or plaques
- Testicular abnormalities like shrinking
- Prostate enlargement or inflammation
- Signs of gynecomastia like enlarged breast tissue
Doctors also evaluate body mass composition, musculoskeletal status and blood pressure during clinical evaluation.
Hormone Laboratory Tests A blood draw is always performed to quantify total testosterone concentration for comparison to standardized reference ranges based on age brackets.
Common additional lab work ordered includes:
- LH and FSH to check pituitary signalling
- Thyroid function (TSH)
- Iron levels and red blood cell counts
- Metabolic panel testing blood sugar, cholesterol and vitamin D
Salivary or urine testosterone assays are now gaining support as non-invasive alternatives. However, blood continues to qualify as the clinical gold standard.
Now what can be done when numbers confirm deficient testosterone is perpetuating digestive troubles like constipation?
Medical Treatments for Low Testosterone
Working alongside a trained hormone therapist or men’s reproductive health specialist, there are two mainstream approaches to resolving low T:
- Testosterone Replacement Therapy (TRT) – If extreme testosterone deficiency significantly impacts daily quality of life, TRT can effectively restore balance. This involves the direct introduction of bioidentical (synthetic) testosterone into circulation via:
- Intramuscular injections (cypionate, enanthate, propionate esters)
- Transdermal skin gels/solutions
- Subcutaneous pellets implanted under fat layers
- Secondary Hypogonadism Treatment – In certain cases like pituitary disease, augmenting underlying LH/FSH signals prompting testes to resume natural production may be preferable over lifelong testosterone supplementation.
Available prescription gonadotropin medications include:
- Human chorionic gonadotropin (hCG)
- Recombinant LH or FSH
- Synthetic GnRH pumps
Both approaches require consistent monitoring via labs and dose titration in response to patient symptoms and total/free T ratio optimization.
Noticeable control over constipation and other gastrointestinal complaints typically manifests within weeks to months of balancing hormones back to optimal zones. Now what about complementary natural tactics?
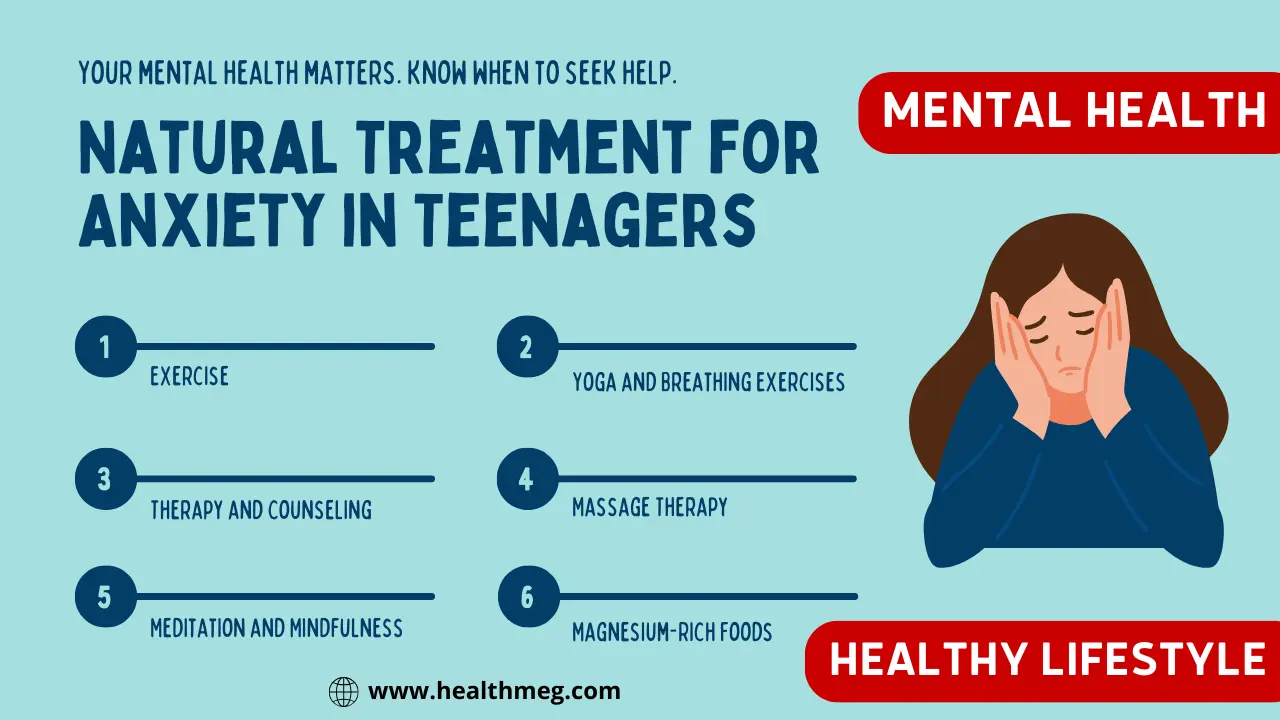
Lifestyle Changes Proven to Help
Clinical studies confirm wide-ranging lifestyle measures beneficially impact low testosterone and digestive dysfunction simultaneously:
- Cut Added Sugar and Refined Carbs – Reducing blood sugar spikes and inflammation helps normalize hormone levels and “leaky gut.”
- Up Nutrient Density – Emphasize gut-healing foods high in zinc, magnesium and vitamin D like oysters, nuts, seeds and quality animal proteins.
- Take Key Supplements – Digestive enzymes, probiotic blends, berberine and bovine colostrum supplements facilitate intestinal healing.
- Reduce Stress – Cortisol directly opposes testosterone production and health. Practice relaxing habits like meditation, yoga, massage and forest bathing.
- Optimize Sleep Hygiene – Testosterone concentration dependably surges overnight if sleep quality is sound, consistent and ample.
- Increase Activity Levels – Aerobic and strength training drives circulation while reducing hormonal abnormalities related to excess body fat storage.
Conclusion
extensive scientific evidence highlights low testosterone as a common yet overlooked culprit perpetuating sudden adult onset constipation. Testing hormone levels while pursuing integrated treatment approaches focusing on restoring balance ties directly to resolving discomfort through sustainable improvement of metabolic, muscular and microbiome functions supporting healthy digestion and waste elimination. Discussing your symptoms with a knowledgeable men’s health specialist remains imperative.
People Also Ask (FAQs)
Confused why gastrointestinal distress suddenly develops in middle age? Unsure about viable solutions for easing this frustrating linked symptom?
Q1: Is low testosterone linked to constipation?
Yes. Extensive research now confirms that declining testosterone levels commonly manifest in the form of gastrointestinal dysfunction—frequently constipation—due to reduced intestinal contractions, nerve sensitivity and muscle strength over time.
Q2: Does Boosting testosterone help with constipation?
Absolutely. Restoring deficient testosterone levels promptly back into healthy ranges via prescription medications, lifestyle tactics or often through combined avenues reliably alleviates associated digestion complaints like constipation.
Q3: Why does low testosterone cause constipation?
This key sex hormone directly maintains regular bowel movements by stimulating intestinal contractions, governing muscle integrity, regulating inflammation and shaping microbiome populations. Declining concentration hampers these processes—slowing motility.
Q4: How are low testosterone and gut health connected?
The intricate gut-testes axis describes the interdependent relationship between sex hormones and digestive functioning. Imbalances from either side exacerbate the other. Optimizing circulation and microbiome diversity counteracts poor nutrient absorption driving low testosterone.
Q5: What digestive problems are linked to low testosterone?
Constipation constitutes the most extensively documented gastrointestinal complaint in modest to severe testosterone deficiency. Additionally, symptoms like diarrhoea, bloating, cramping, SIBO, slow motility, haemorrhoids and IBS often arise as well.
Q6: What causes low testosterone-related constipation?
Root causes include declining strength of intestinal smooth muscles, reduced nerve conductivity, gut lining inflammation, microbiome disruption, poor hydration and overactive water reabsorption in the colon—all regulated by testosterone concentration to some degree.
Q7: How can you stop testosterone-induced constipation?
Eliminating underlying low T is key. This is achievable through prescription testosterone replacement therapy or secondary hormonal medications. Complementary diet, lifestyle and stress-reducing interventions also prove beneficial.
Q8: What foods reduce testosterone causing constipation?
Emphasize probiotic and prebiotic fibre sources like kefir, kimchi, kombucha, bone broth, onions, garlic, bananas, flax and oats. Keep hydrated. Add magnesium from spinach, avocado and nuts which relaxes muscles. Reduce dairy and meat temporarily if needed.
Q9: What natural supplements counteract low testosterone constipation?
Digestive enzymes, psyllium husk, aloe vera, triphala, glutamine, dandelion, omega oils and natural probiotics in supplement form accelerate waste transit and healing while lowering inflammation simultaneously.
Q10: Should I take probiotics with low testosterone?
Absolutely, yes. Supportive research concludes that daily probiotic supplementation effectively combats gastrointestinal symptoms induced by declining testosterone like constipation while balancing inflammatory gut flora.
Q11: Do testosterone boosters relieve constipation?
Indirectly, yes. Herbal blends containing Tongkat ali, shilajit, zinc, boron and DHEA serve to gently augment declining testosterone levels into more optimal ranges—stabilizing many low T symptoms like constipation in the process.
Q12: What prescription medications help low T constipation?
Injectable, oral and transdermal testosterone replacement preparations reliably resolve hormone deficiency-induced constipation for most patients. Alternatively, secondary pituitary gonadotropin drugs in certain cases stimulate natural production.
Q13: Do laxatives help low testosterone constipation?
Sometimes initially but not for long-term reliance. These stimulate unnatural rapid bowel movements but possess no capacity to resolve the underlying testosterone loss perpetuating disordered motility.
Q14: What blood tests diagnose low testosterone levels?
Checking total testosterone blood serum concentration remains the clinical gold standard diagnostic. Additional labs like free T, SHBG, LH, FSH, PSA and metabolic biomarkers also help specify the catalyst, severity and personalized treatment approach.
Q15: How common is low testosterone in ageing men?
After 30, testosterone gradually depletes at a steady rate of 1 percent annually. Around 2 percent of men in their 40s suffer clear hormone deficiency expanding to 50 percent of those in their 80s. Contributing illness and lifestyle factors also drive prevalence higher through middle age.
Q16: At what testosterone level is constipation common?
Every man experiences symptoms differently but most gastrointestinal issues including constipation emerge once circulating total t levels consistently register below 400-500 ng/dL —sometimes higher or lower among individuals depending on sensitivity.
Q17: What testosterone concentration is too low?
Endocrinology experts classically define true biochemical testosterone deficiency upon total blood levels sinking persistently below 300 ng/dL coupled with worsening symptoms impairing quality of life like constipation. However, depending on age, the optimal ranges for feeling best extend between 500-900 ng/dL for adult men.
Q18: How do doctors test testosterone levels at home?
Now physicians can prescribe convenient at-home saliva or dried blood spot test kits which users self-collect and then mail into licensed clinical laboratories for analysis rather than visiting phlebotomy labs. However, serum blood continues to rank as the most accurate assay.
Q19: Can constipation cause low testosterone?
While the majority of research focuses on declining testosterone-inducing constipation, another school of thought credits chronic gastrointestinal distress as detrimental to anabolic hormone balance. Some data concludes constipation signifies impaired gut-testes signalling. Resolving digestion kinks may support production.
Q20: Can gut bacteria increase testosterone?
Extensive investigation now confirms that nourishing a thriving, diverse intestinal microbiome marked by favourable Firmicutes species directly facilitates bodily testosterone availability by converting precursor molecules into active forms.
Q21: Does probiotic yogurt help low testosterone?
Potentially yes. Alongside supporting live microbe supplementation, choosing traditional unpasteurized strains of yogurt offers proven prebiotic substrates while reducing gut lactose intolerance exacerbating low T. However quality remains paramount for benefit.
Q22: What digestive enzymes are low in T?
Foremost deficiencies centre upon decreased bile acid and microbiome-derived enzyme production—namely alpha-galactosidase, glucocerebrosidase and beta-galactosidase—required to break down complex carbohydrates. This causes dysbiosis and malabsorption.
Q23: How can I increase stomach acid naturally?
Relax during meals, chew thoroughly, sip organic apple cider vinegar, take concentrated betaine HCL, and drink kefir and bone broth. Emphasize vitamin C intake from camu camu berry and alkalizing magnesium, zinc, and chromium. Consider digestive bitters like gentian.
Q24: Do testosterone injections help digestion?
For men genuinely exhibiting a testosterone deficiency—total levels under 300 ng/dL—commencing testosterone injection or gel preparations often rapidly stabilizes digestive dysfunction stemming from hormone imbalance including stubborn constipation.
Q25: How often should injections be given for low Testosterone?
Testosterone injections embedded within muscular tissue for absorption generate dramatic peaks and plunges. This necessitates a strict protocol of 100-200 mg doses every 7-14 days. More frequent or lower doses smooth out cycling. Transdermal and pellet routes enable steadier circulation.
Q26: Are pellets or injections better for low Testosterone?
Both modalities succeed in elevating total and free testosterone ratios. Biodegradable pellet implants placed underneath the skin every 4-6 months promote remarkably stable concentration due to slow release while bypassing liver breakdown. Painless injections afford patients more direct control over varying dose needs.
Q27: How long do testosterone pellets last?
The implants steadily bio-erode to furnish active testosterone for about four to six months on average. Younger men may clear through them quicker while less physiologically robust 65+ year olds can experience symptom relief exceeding nine months before requiring replacement.