Introduction
The most recent data indicates that in 2021, a record 9,234 liver transplants were performed in the United States. This is a significant increase from the 8,000 liver transplants performed in 2017, providing a second chance at life for those with end-stage liver disease. However, the road to recovery after a transplant can be filled with significant physical, emotional and mental health challenges that many recipients feel unprepared to handle. Studies indicate a high prevalence of psychiatric issues post-transplant, with up to 60% of patients experiencing disorders like depression, anxiety, substance abuse and sleep disturbances in the months and years following surgery.
This article provides an in-depth look at the common mental health problems arising after a liver transplant. It discusses the need for comprehensive long-term clinical care to help recipients successfully adapt to their new normal, research on how mental illness can negatively impact outcomes, ongoing cognitive concerns, the importance of social support systems, and expert advice for coping with psychological struggles. The goal is to bring awareness to these quality-of-life challenges which are rarely talked about, provide actionable solutions and support for those struggling, and give medical professionals insight into better caring for their patients’ total wellbeing.
Let’s understand the mental problems after liver transplant a person can have in this comprehensive guide.
Do read the People Also Ask (FAQs) about this topic.
Key Takeaway
- Major issues include high rates of depression, anxiety disorders, PTSD, substance abuse relapse and sleep disturbances resulting from gruelling recovery, medication side effects, loss of autonomy plus pre-existing conditions exacerbated by traumatic surgery. Proper psychiatric treatment and social support prove critical.
- Up to 60% of liver transplant recipients experience psychiatric issues like depression, anxiety, and sleep disturbances after surgery. Comprehensive long-term clinical care is crucial for helping them adapt.
- Substance abuse relapse is a major concern, with 20% reverting to heavy drinking post-transplant, jeopardizing organ survival. Vigilant monitoring and treatment plans are necessary.
- Feelings of depression affected 30-60% of recipients in the first few years and stemmed from medication side effects, loss of autonomy, self-image issues and grief. This can reduce survival rates if unaddressed.
- Sleep disorders like insomnia arise in 42-65% of patients due to immunosuppressant side effects, corticosteroids, anxiety, or pain medications. Focusing on sleep hygiene and treatments helps regain normal sleep.
- Up to 15% of recipients exhibit PTSD symptoms like flashbacks and avoidance behaviours due to the trauma of surgery and experiences in the ICU. Counselling helps patients process these memories.
Common Mental Problems After Liver Transplant
Research indicates a significant prevalence of psychiatric conditions among liver transplant recipients in the initial years following surgery.
A 2023 study published in BMC Gastroenterology reported that nearly 30% of liver transplant recipients had comorbid psychiatric disorders. The most frequently diagnosed conditions included insomnia, delirium, major depressive disorder, adjustment disorder, and anxiety disorder.
Meanwhile, a 2022 study in Middle East Current Psychiatry evaluated cognitive functions in patients with end-stage liver disease (ESLD) before and after liver transplantation. The study reported a significant improvement in cognitive functions 3 months post-transplantation.
Furthermore, a 2021 study in Frontiers in Psychiatry found that psychological distress was prevalent in organ transplant recipients during the COVID-19 pandemic. The prevalence of depression, anxiety, insomnia, and PTSD in organ transplant recipients was 13.4%, 6.9%, 11.8%, and 30.5%, respectively.
These studies highlight the complex interplay of various factors contributing to the mental health of liver transplant recipients. These include functional impairments, financial concerns, side effects of immunosuppressant medications, and more.
Substance Use Disorders
Substance Use Disorders Patients with chronic liver disease often have a history of substance abuse, including excessive alcohol consumption or drug use. A liver transplant can serve as a catalyst for sobriety, but the risk of relapse remains a significant concern. Research suggests that nearly 20% of liver transplant recipients revert to heavy drinking post-transplant, which can compromise the survival of the new organ.
Substance abuse not only poses a direct threat to liver health but also exacerbates mental health conditions such as depression and anxiety. It can undermine the support networks crucial for recovery and often leads to non-adherence to post-transplant protocols. A study found that illicit drug use after a liver transplant was associated with a 36% increase in mortality risk.
In light of these findings, medical professionals stress the importance of vigilant monitoring for signs of substance misuse in liver transplant recipients. They also underscore the necessity of having treatment plans ready for those at higher risk.
Depression
Feelings of depression affect an estimated 30-60% of liver recipients in the first few years following surgery. There are multiple factors behind these numbers:
Physical Side Effects: Medications like corticosteroids can directly cause mood changes. Fatigue during recovery also hampers participation in enjoyable activities.
Loss of Control: No longer feeling autonomous combined with relying on family for basic needs brings emotional turmoil.
Self-Image Struggles: Changes in appearance from scars or weight gain/loss often damage a patient’s self-confidence.
Grief: End-stage liver disease diagnosis and arduous transplant process involve much loss to process.
Research consistently associates post-transplant depression with reduced survival rates, decreased ability to return to work, diminished social functioning, and lower energy levels. Approaches such as seeking counselling, joining liver transplant support groups, and using certain antidepressants have been found to assist many in navigating this challenging adjustment period.
Sleep Disorders
Research indicates that 42-65% of liver recipients experience sleep disturbances post-transplant, which can negatively impact mental health. Insomnia is most common, presenting as trouble falling asleep, frequent nighttime awakenings or early morning waking.
Causes include side effects of immunosuppressants, corticosteroids causing restless legs or anxiety disrupting the ability to wind down. Sleep apnea triggered by pain medications and metabolic changes also occurs. Effects of poor sleep compound exhaustion and moodiness already present while healing.
Doctors suggest focusing on sleep hygiene by sticking to set sleep/wake times, limiting naps, avoiding screens before bed and creating an optimal rest environment. Antihistamines, tricyclic antidepressants, cognitive behavioural therapy or CPAP machines also help many regain normal sleep patterns.
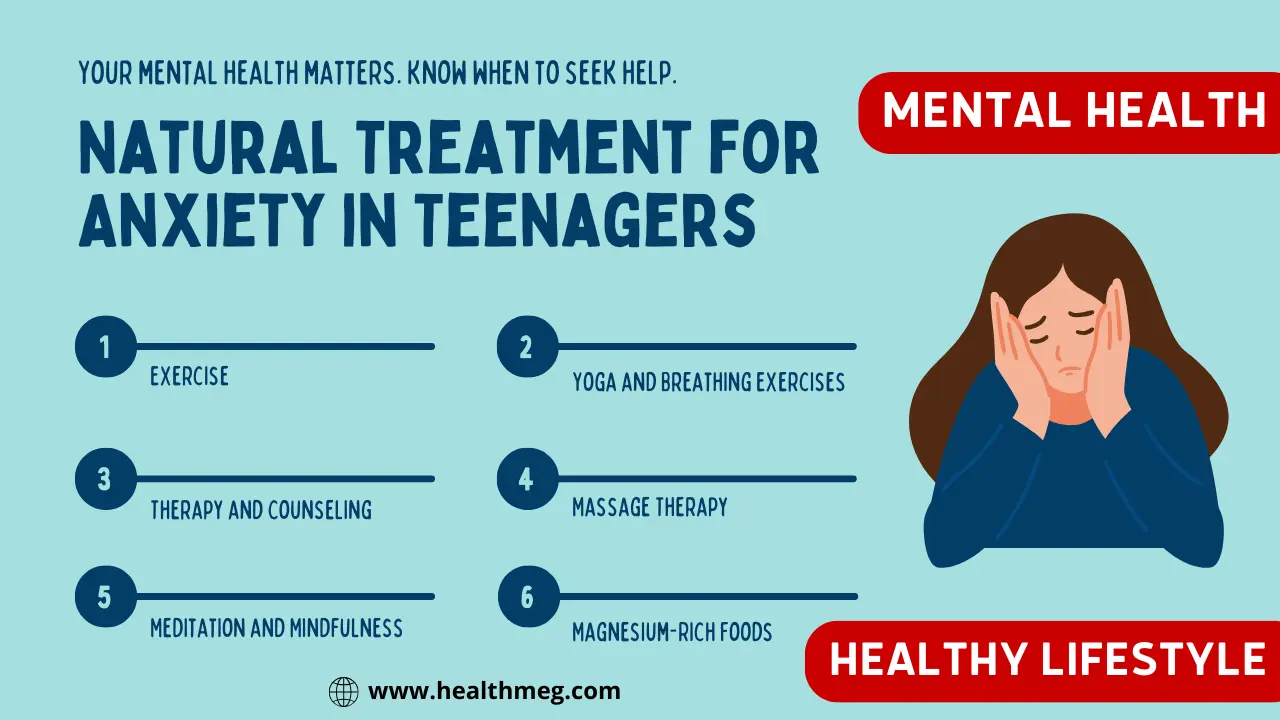
Anxiety Disorders
Post-transplant anxiety is a common occurrence, with studies indicating that up to 20% of kidney recipients, 30% of liver recipients, and 63% of heart recipients are affected, especially in the first year. The fear of organ rejection, medication side effects, and limitations in functioning all contribute to this anxiety.
In the early stages post-discharge, anxiety tends to revolve around medical uncertainties, while later stages see a shift towards concerns related to financial issues, employment, and social reintegration. Panic attacks, generalized anxiety, and adjustment disorders with anxiety are prominent features.
Relaxation techniques, cognitive behavioural approaches, and if necessary, anti-anxiety medications can help patients manage their anxiety. It’s also important for doctors to emphasize the need for patients to have realistic expectations post-transplant. Understanding that temporary setbacks are possible can help patients adapt to their journey.
Post-Traumatic Stress Disorder
A liver transplant ranks as a significantly traumatic life event for most patients. Facing the hardship of end-stage liver failure and then undergoing major surgery creates noticeable emotional scarring even when physically cured.
According to the study up to 15.1% of solid-organ transplant recipients, including liver recipients, exhibit symptoms of PTSD. These symptoms include flashbacks, avoidance behaviour, and hypervigilance. The stressful experiences in the ICU and hospital, post-surgical pain, and the reduction in social support after discharge are key contributors to these symptoms.
Counselling helps patients process memories to lessen their negative emotional charge. Doctors also underline that temporary regression in mood or anxiety during trigger events like anniversaries or future procedures is normal.
The Need for Long-Term Post-Transplant Clinical Care
Importance of Long-Term Care
The barrage of mental health disorders arising after liver transplants confirms comprehensive long-term clinical care is essential. Unlike resolving an acute medical condition, receiving a donor organ represents an ongoing lifestyle change never allowing recipients to be discharged from oversight.
Ongoing stress around maintaining transplant protocols mandates access to psychologists, psychiatrists, social workers and vocational rehabilitation counsellors. This multidisciplinary approach identifies emotional issues early before spiralling into a lack of self-care compliance or addiction relapse threatening the transplant’s survival. It also facilitates the critical shift from passive patient to empowered self-manager vital for persevering in the journey ahead.
Role of Healthcare Professionals
Transplant centres strive to ensure a smooth handoff of care from the surgical team to long-term providers familiar with the challenges that follow. Primary care doctors coordinate referrals to specialists while case managers connect patients to financial assistance programs or community resources.
Mental health at follow-ups should be as high a priority as tracking lab results or medication side effects. Incorporating screenings by having patients complete valid psychiatric questionnaires allows problems to be caught early. Questions on substance use, self-care adherence and participation restrictions also help determine who needs extra support.
Adherence to Recommendations
Lifelong adherence to post-transplant recommendations can seem a burdensome chore eroding recipients’ quality of life. Mental health thus directly impacts compliance levels, especially medication adherence. Studies demonstrate patients with depression or cognitive complaints begin missing doses sooner without the cognitive capacity to manage complex regimens.
That’s why psychiatric care plans must be established to stabilize mental health issues and reinforce the necessity of protocols for long-term outcomes. Support groups also provide empathy and peer understanding that expert advice alone often cannot achieve to inspire sticking to the plan.
Association of Depression with Poorer Post-Transplant Outcomes
Research Findings
The high prevalence of psychiatric conditions post-transplant means examining their impact on measurable health outcomes is crucial. Multiple studies have found a significant link between mental illness, especially depression, after liver transplant surgery and reduced survival rates or organ rejection.
A study titled “Comorbid psychiatric disorders and long-term survival after liver transplantation in transplant facilities with a psychiatric consultation-liaison team: a multicenter retrospective study” found that comorbid psychiatric disorders, including depression, negatively affect the survival rate of liver transplant recipients. This study monitored over 1006 transplant recipients and found that 29.2% had comorbid psychiatric disorders.
Another study titled “Psychological Distress and Its Association With Quality of Life in Organ Transplant Recipients During COVID-19 Pandemic” found that the prevalence of depression in organ transplant recipients was 13.4%2. The study followed organ transplant recipients during the COVID-19 pandemic and found that those with depression had significantly lower scores in all eight dimensions of Quality of Life compared with participants without depression.
Implications
The evidence clearly demonstrates that properly addressing mental health concerns, including depression, early after discharge provides tangible physical health benefits further down the road. Failure to resolve destructive thought patterns leaves recipients less capable of managing the rigorous self-care responsibilities transplant requires.
These research conclusions should prompt transplant hospitals to devote more resources towards building comprehensive psychiatric frameworks. Stress reduction programs, easily accessible counselling teams, and support staff fully trained in mental health first aid all help recipients reach positive outcomes. No patient should find their second chance at life hampered by treatable mood disorders. Employers and insurance networks must also better recognize the importance of mental health in post-transplant care.
Cognitive Issues Following Transplant
After recovering physically from a liver transplant procedure, many recipients expect their lives will largely return to normal. However, the trauma of extensive surgery coupled with psychiatric medications can often leave lasting cognitive impairment noticeably reducing quality of life.
Potential for Cognitive Issues
Researchers hypothesize the accumulation of neurological insults before and after transplantation likely explains ongoing memory, concentration and processing problems. The effects of liver failure create physiological vulnerability within the brain while surgery itself threatens the oxygen supply causing regional damage.
Heavy regimen immunosuppressant drugs also seemingly exert neurotoxic effects through mechanisms still being explored. Evaluating cognitive function both before and longitudinally after transplantation demonstrates while many domains improve once liver function is restored, noticeable deficits frequently linger long-term.
Types of Cognitive Issues
The most prominent cognitive complaints reported by liver recipients include:
- Memory loss
- Difficulty concentrating for long periods
- Impaired executive functioning makes it harder to multitask or filter competing stimuli
- Slower information processing speed leads to frustration
- Reduced vocabulary diversity suggests compromised verbal recall
Causes are multifactorial ranging from normal aging exacerbated by years of liver disease to depression/anxiety severing focus. Medications like prednisone, antibiotic regimens and sedative anaesthetics during surgery also negatively impact cognition.
Frustration frequently accompanies emerging cognitive problems after liver transplant surgery since recipients expect their ordeal to end once recovering physically. Admitting mental capacity seems continuously hampered even if life-saving proves emotionally taxing.
Management Strategies
While research on cognitive rehabilitation specific to post-transplant patients remains limited, general techniques for managing impairment exist:
- Prescribing psychostimulants to enhance concentration and motivation
- Compensating for memory loss using external tools like calendars, reminders, note-taking
- Reducing multi-tasking to avoid overstimulation
- Engaging in brain training games and apps to promote processing speed
Some transplant centres also offer focused cognitive therapy incorporating stress reduction, mental exercises, coping method development and psychotherapy for emotional aspects like self-esteem injury over diminished skills.
Maintaining follow-up screenings for cognitive function allows problems to be caught and managed early before they severely impact work performance or important relationships.
Personal Experiences and Case Studies
- Post-transplant Psychosocial and Mental Health Care of the Liver Recipient: This research highlights the mental health challenges that liver transplant recipients can face following the procedure. It underscores the importance of long-term clinical care post-transplant, particularly for patients experiencing cognitive impairment or depression.
- Post-Transplant Mental Health & Well-being: Q&A with Shelia Jowsey-Gregoire, M.D.: In this insightful Q&A, Dr. Shelia Jowsey-Gregoire, a psychiatrist at Mayo Clinic’s transplant centre, discusses the emotional and psychological transitions that transplant patients undergo. She talks about the variety of emotions that transplant patients can experience and suggests tools for adjusting to life after transplant.
- Comorbid psychiatric disorders and long-term survival after liver transplantation in transplant facilities with a psychiatric consultation-liaison team: a multicenter retrospective study: This study reveals that comorbid psychiatric disorders, including depression, can negatively impact the survival rate of liver transplant recipients.
- Mental health in children with living donor liver transplantation: a case-control study: This study compares the mental health of pediatric liver transplant patients with healthy children. It found that patients after liver transplantation were more prone to emotional problems, hyperactivity, and peer problems. The study also identified parental mental health, physical activity, and family environment as factors associated with the mental health of pediatric liver transplant patients.
That’s why guidelines recommend completing psychiatric treatment programs and stricter screening for risk factors like substance abuse before approval. Transplant programs also increasingly require demonstrating engagement in support communities for extra preparation and accountability.
The Role of Family and Social Support
Importance of Support Systems
Maintaining reliable support systems is arguably vital to effectively managing liver transplantation’s lifelong mental rigours. Whether enduring years of illness or the acute recovery phase, patients universally highlight how social connections providing encouragement and tangible aid alleviate the emotional tolls of adjusting.
Studies demonstrate transplant recipients with higher perceived family/friend support experience less depression and anxiety at all points of the journey. They display a better understanding of medication protocols, follow post-discharge instructions more closely and attend appointments reliably. Feeling cared for and understood fundamentally sustains motivation on especially difficult days.
Equally, those reporting insufficient social support or isolation following surgery exhibit sharply higher rates of PTSD, suicidal thoughts and substance abuse relapses. Emotional vulnerability left untended too often translates into self-destructive actions undermining their second chance.
Role of Family and Friends
For married recipients or those in steady relationships, partners represent an invaluable pillar when strength falters. Research documents that patients overwhelmingly lean hardest on spouses through every mental and physical valley from waiting lists to discharge. Handling household burdens or offering encouragement during low moods proves essential.
Wider family and close friends further cement this circle of care by providing meals, transportation assistance and often financial help. Having personal confidants who intimately understand patients’ journeys helps normalize complaints to doctors that seem trivial to those never sick. Maintaining a digital journal about the process also keeps faraway loved ones engaged in progress.
Building a Support System
For recipients lacking innate support networks either through isolation or strained relationships, cultivating community post-transplant grows increasingly vital. Besides easing logistical burdens, transplant centres say most individuals’ mental health feedback suggests that simply feeling heard by those who “get it” offers emotional comfort.
In-person and online support groups thus help participants swap stories to establish they aren’t alone working through disappointment spells or down days. Counsellors advise investing time into forging social bonds even if difficult without natural circumstances creating connections.
Local non-profit organizations, hospital community partners and places of worship also provide meals, rides and heartening messages if recipients take that first step in reaching out. You never know what care arises until asking.
Expert Advice for Coping with Mental Health Post-Transplant
Navigating the emotional landscape after an organ transplant can be challenging. Here are some expert-recommended strategies to help manage mental health post-transplant:
- Emotional Coping Mechanisms: Post-transplant patients may experience a range of emotions, including guilt, disappointment, and family-related issues. Experts suggest seeking professional help if these feelings become overwhelming. (WebMD)
- Maintaining a Positive Attitude: According to Dr Shelia Jowsey-Gregoire, a psychiatrist at Mayo Clinic’s transplant centre, maintaining a positive attitude, establishing a support network, facing fears, problem-solving, helping others, having a sense of humour, being flexible, and attending to physical well-being is crucial for adjusting to life after transplant. (Mayo Clinic)
- Engaging in Relaxing Activities: Finding hobbies and activities that you enjoy can help manage emotions post-transplant. This could include meditation, deep breathing exercises, journaling, or setting small, achievable goals. (Kidneyfund)
These strategies underscore the importance of mental health in the recovery process post-transplant. By recognizing and addressing these issues early, patients can improve their quality of life and overall well-being.
Conclusion
The multitude of psychiatric conditions arising after liver transplantation like depression, anxiety and post-traumatic stress too frequently get dismissed as incidental concerns. Yet substantial research demonstrates these mood disorders’ dangerous implications ranging from sabotaging post-surgical compliance to directly reducing recipient survival rates.
That’s why taking proactive ownership of mental health through counselling, peer support, cognitive coping strategies and more proves so essential following hospital discharge.
People Also Ask (FAQs)
Q) Do personalities change after an organ transplant?
A) Personality changes can occur after an organ transplant due to the traumatic nature of major surgery coupled with psychiatric medication side effects. Mood shifts like depression, anxiety, and irritation are common but typically improve over the first year.
Q) What causes mental confusion after a liver transplant?
A) Mental confusion after a liver transplant often results from anaesthetic medications, ICU delirium triggered by interventions or electrolyte imbalance, immunosuppressant drug toxicity, infections, and residual effects of liver failure.
Q) Can a liver transplant affect the brain?
A) Yes, liver transplants can affect the brain. Anti-rejection medications may have neurotoxic effects. Hypoxia during surgery, pain meds, metabolic changes and stress hormone shifts also impair cognition. Pre-transplant hepatic encephalopathy may not fully resolve.
Q) What are the psychological effects of liver transplants?
A) Common psychological effects of a liver transplant include depression, anxiety over organ rejection, post-traumatic stress, frustration over new limits, body image issues, lowered self-esteem, relationship strain, and substance abuse relapse risk.
Q) What are the psychological effects of organ transplants?
A) Typical psychological effects of any type of organ transplant include high stress adapting to lifelong medication protocols and fears over organ failure taking a toll on mental health. Personality shifts are also common along with grief over the loss of a former life before chronic illness necessitated transplant.